Obstructive sleep apnoea (OSA) is a common sleep disorder, which has been linked to many adverse health outcomes including excessive sleepiness, impaired quality of life including daytime alertness, cognitive function, mood, motor vehicle crashes and cardiovascular events. Positive airways pressure (PAP) is the primary treatment modality.
Obstructive sleep apnoea (OSA) is a common sleep disorder, which has been linked to many adverse health outcomes including excessive sleepiness, impaired quality of life including daytime alertness, cognitive function, mood, motor vehicle crashes and cardiovascular events. Positive airways pressure (PAP) is the primary treatment modality.
Use of CPAP in people with OSA to improve daytime sleepiness, sleep-related quality of life and modest lowering of blood pressure, particularly nocturnal systolic blood pressure.
A 2019 systematic review commissioned by the American Academy of Sleep Medicine found that CPAP resulted in a reduction in sleepiness, blood pressure, and motor vehicle accidents, compared with no treatment in people with OSA. CPAP also improved sleep-related quality of life. The effectiveness of CPAP in reducing cardiovascular events and all-cause mortality in OSA was inconclusive.1
Precautions
Ensure that prior to treatment of OSA with CPAP, a diagnosis of OSA has been established using objective sleep apnoea testing.
Adverse effects
Side effects that have been reported with CPAP include nasal dryness/irritation, dry mouth, sore throat and sinus infection.1
- Poor adherence (usually defined as less than of 4 hours in a 24-hour period) with CPAP limits its effectiveness. Technological advances have improved the fit and comfort of the masks but regular follow-up and troubleshooting are needed.1, 2
- Mandibular advancement devices may be an alternative to CPAP.2
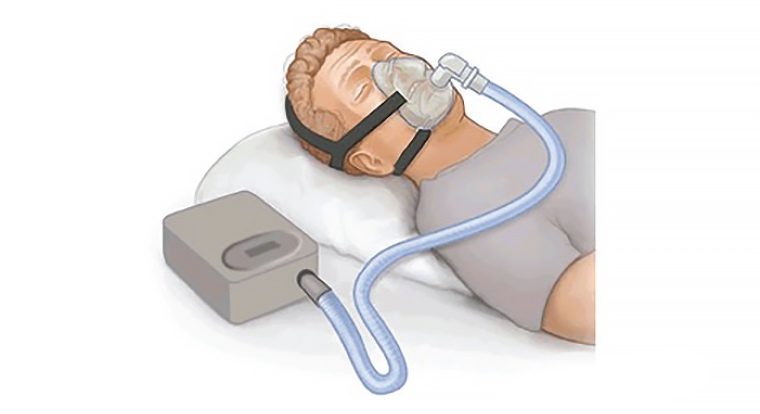
CPAP is the most efficacious therapy to treat OSA (Figure 1).2 Neurocognitive benefits noticed by patients may not always closely correlate with improvements detected during polysomnography.2 Despite this, a linear improvement in both subjective and objective daytime sleepiness in patients with severe OSA has been found when CPAP is used up to seven hours per night.2
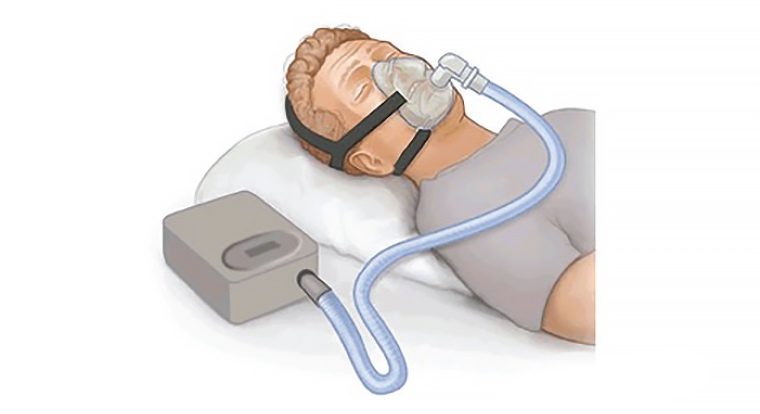
Figure 1. A CPAP device fitted to provide positive pressure to nasal and oral cavities during sleep.
‘CPAP.png’ by PruebasBMA is licenced under CC BY-SA 3.0. The original image can be found at https://commons.wikimedia.org/wiki/File:CPAP.png [Accessed 17 February 2024].
Public funding of CPAP varies by state and territory in Australia. The cost of the CPAP, mask and other accessories has been estimated to be over $1500. Access to CPAP is via a home or laboratory-based sleep study. The pathway to having a sleep study can be through referral to a sleep or respiratory specialist or via direct referral from the GP, when the following Medicare criteria are met: A high pre-test probability of symptomatic, moderate-severe OSA is confirmed by a Epworth Sleepiness Scale (ESS) score ≥ 8, and OSA50 score ≥5 or STOP-Bang score ≥3.
Consumer resources
Other resources
An Alaska license plate search lets you find information about a vehicle using its license plate number. This search can provide details such as the vehicle’s make, model, year, and registration status. You can conduct a search through the Alaska Tax Commission or various third-party websites. Personal owner information is protected by privacy laws. This service is useful for verifying vehicle details, researching a car’s history, or investigating incidents.